Patient information about the coronavirus
written by
Coronavirus (COVID-19)
A coronavirus outbreak started in December 2019 in the Wuhan region of China. The virus can cause the disease COVID-19. The name “coronavirus” comes from the crown-like projections on their surfaces. “Corona” in Latin means “halo” or “crown”. Among humans, coronavirus infections most often occur during the winter months and early spring. Since then, the virus has spread to other countries, both in and outside Asia, leading the World Health Organization (WHO) to declare this as a pandemic.The following information is adapted from health institutions, governmental organizations, research results and news agencies.
Coronavirus symptoms
- Fever
- Cough
- Shortness of breath or difficulty breathing
- Tiredness
- Aches
- Runny nose
- Sore throat
- Sudden loss of taste or smell
Leave a review now to share with others what your symptoms of this coronavirus are.
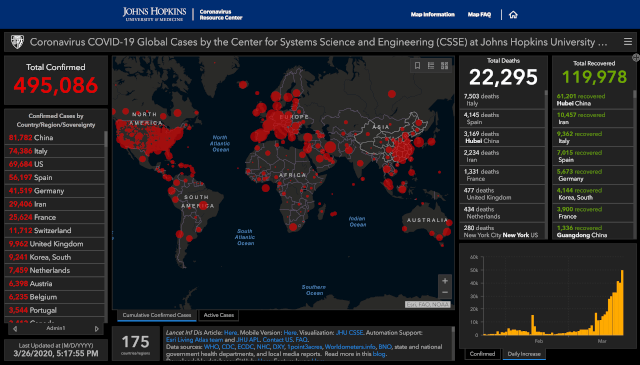
Seriousness
We still do not know whether the coronavirus is more serious than a common flu. The official figures for the moment do not seem very disturbing. But we do not know exactly how much delay there is in the data and whether there is underreporting and how large it is. The point is that it is a new virus. It is then important to get very detailed information to determine exactly how dangerous the virus is. More information is needed about the spreading of the virus.
This virus infects people of all ages. However, evidence to date suggests that two groups of people are at a higher risk of getting severe COVID-19 disease. These are older people (that is people over 60 years old) and those with underlying medical conditions (such as cardiovascular disease, diabetes, chronic respiratory disease and cancer). The risk of severe disease gradually increases with age starting from around 40 years. It’s important that adults in this age range protect themselves and in turn protect others that may be more vulnerable.
Contagiousness
The disease is transmitted from person to person. It is currently assumed that one sick person can infect an average of 2 other people. The sicker a person is, the more it spreads the virus.
Prevent contamination
Wash your hands frequently
Regularly and thoroughly clean your hands with an alcohol-based hand rub or wash them with soap and water.
Why? Washing your hands with soap and water or using alcohol-based hand rub kills viruses that may be on your hands.
Maintain social distancing
Maintain at least 1 meter (3 feet), but preferably 2-3 meter (6-10 feet) distance between yourself and anyone who is coughing or sneezing.
Why? When someone coughs or sneezes they spray small liquid droplets from their nose or mouth which may contain the virus. If you are too close, you can breathe in the droplets, including the COVID-19 virus if the person coughing has the disease.
Avoid touching eyes, nose and mouth
Why? Hands touch many surfaces and can pick up viruses. Once contaminated, hands can transfer the virus to your eyes, nose or mouth. From there, the virus can enter your body and can make you sick.
Practice respiratory hygiene
Make sure you, and the people around you, follow good respiratory hygiene. This means covering your mouth and nose with your bent elbow or tissue when you cough or sneeze. If you use a tissue dispose it afterwards.
Why? Droplets spread virus. By following good respiratory hygiene you protect the people around you from viruses such as cold, flu and COVID-19.
If you have fever, cough and difficulty breathing, seek medical care early
Stay home if you feel unwell. If you have a fever, cough and difficulty breathing, seek medical attention and call in advance. Follow the directions of your local health authority.
Why? National and local authorities will have the most up to date information on the situation in your area. Calling in advance will allow your health care provider to quickly direct you to the right health facility. This will also protect you and help prevent spread of viruses and other infections.
Stay at home if you begin to feel unwell, even with mild symptoms such as headache and slight runny nose, until you recover. Why? Avoiding contact with others and visits to medical facilities will allow these facilities to operate more effectively and help protect you and others from possible COVID-19 and other viruses.
Common questions
How long can the coronavirus stay airborne? I have read different estimates.
A study done by National Institute of Allergy and Infectious Diseases' Laboratory of Virology in the Division of Intramural Research in Hamilton, Montana helps to answer this question. The researchers used a nebulizer to blow coronaviruses into the air. They found that infectious viruses could remain in the air for up to three hours. The results of the study were published in the New England Journal of Medicine on March 17, 2020.
How long can the coronavirus survive on surfaces?
A recent study found that the COVID-19 coronavirus can survive up to four hours on copper, up to 24 hours on cardboard, and up to two to three days on plastic and stainless steel. The researchers also found that this virus can hang out as droplets in the air for up to three hours before they fall. But most often they will fall more quickly.
There's a lot we still don't know, such as how different conditions, such as exposure to sunlight, heat, or cold, can affect these survival times.
As we learn more, continue to follow the CDC's recommendations for cleaning frequently touched surfaces and objects every day. These include, for example, counters, tabletops, doorknobs, bathroom fixtures, toilets, phones, keyboards, tablets, and bedside tables.
Is it a seasonal virus?
People regularly become ill with a cold due to a coronavirus and may catch the same one about 4 months later.
This is because coronavirus antibodies do not last for a long time.
Also, the antibodies for one strain of coronavirus may be ineffective against another one.
Is it better to live in warmer climates or colder climates?
From the evidence so far, the COVID-19 virus can be transmitted in ALL AREAS, including areas with hot and humid weather.
There is no reason to believe that cold weather can kill the new coronavirus or other diseases. The normal human body temperature remains around 36.5°C to 37°C, regardless of the external temperature or weather.
Regardless of climate, adopt protective measures if you live in, or travel to an area reporting COVID-19.
The best way to protect yourself against COVID-19 is by frequently cleaning your hands. By doing this you eliminate viruses that may be on your hands and avoid infection that could occur by then touching your eyes, mouth, and nose.
Does a hot bath prevent coronavirus?
Taking a hot bath will not prevent you from catching COVID-19. Your normal body temperature remains around 36.5°C to 37°C, regardless of the temperature of your bath or shower. Actually, taking a hot bath with extremely hot water can be harmful, as it can burn you. The best way to protect yourself against COVID-19 is by frequently cleaning your hands. By doing this you eliminate viruses that may be on your hands and avoid infection that could occur by then touching your eyes, mouth, and nose.
Do vaccines against pneumonia protect you against the new coronavirus?
No. Vaccines against pneumonia, such as pneumococcal vaccine and Haemophilus influenza type B (Hib) vaccine, do not provide protection against the new coronavirus.
The virus is so new and different that it needs its own vaccine. Researchers are trying to develop a vaccine against 2019-nCoV, and WHO is supporting their efforts.
Although these vaccines are not effective against 2019-nCoV, vaccination against respiratory illnesses is highly recommended to protect your health.
Should I avoid ibuprofen when I am ill?
Some French doctors advised against using ibuprofen (or other NSAIDs - a group of painkillers like ibuprofen, naproxen, aspirin…) for COVID-19 symptoms based on reports of otherwise healthy people with confirmed COVID-19 who were taking an NSAID for symptom relief and developed a severe illness, especially pneumonia. These are only observations and not based on scientific studies.
If you start to feel symptoms, it is always best to use paracetamol/acetaminophen instead of ibuprofen, since paracetamol gives far less side effects or interactions than medicines like ibuprofen.
However, if you suspect or know you have COVID-19 and cannot take acetaminophen, or have taken the maximum dose and still need symptom relief, taking over-the-counter ibuprofen does not need to be specifically avoided.
I heard that certain blood pressure medicines might worsen symptoms of COVID-19. Should I stop taking my medication now just in case I do get infected? Should I stop if I develop symptoms of COVID-19?
You are referring to angiotensin converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), two types of medications used primarily to treat high blood pressure (hypertension) and heart disease. Doctors also prescribe these medicines for people who have protein in their urine, a common problem in people with diabetes.
At this time, the American Heart Association (AHA), the American College of Cardiology (ACC), and the Heart Failure Society of America (HFSA) strongly recommend that people taking these medications should continue to do so, even if they become infected.
Drug research
Are chloroquine and hydroxychloroquine effective for treating COVID-19?
Recently, there has been considerable discussion of whether two related drugs — chloroquine and hydroxychloroquine — that have been available for decades to treat other illnesses might also be effective in treating COVID-19.
The drugs are primarily used to treat malaria and several inflammatory diseases, including systemic lupus erythematosus (lupus) and rheumatoid arthritis. No drug is perfectly safe, but these drugs are quite safe when used for just the several days they might be needed to treat COVID-19. They are also cheap, already available at our local drug stores, and relatively free of side effects.
The question, of course, is whether they are effective against the coronavirus that causes COVID-19.
There is strong evidence that both drugs kill the COVID-19 virus in the laboratory dish. The drugs appear to work through two mechanisms. First, they make it harder for the virus to attach itself to the cell, inhibiting the virus from entering the cell and multiplying within it. Second, if the virus does manage to get inside the cell, the drugs kill it before it can multiply.
But do the drugs work in people with COVID-19?
Many studies are underway to get an answer to this question, but as of March 24, 2020, only two have issued preliminary results.
One report, published in February 2020, claimed that chloroquine had been used in more than 100 patients in China who had COVID-19. The scientists stated that their results demonstrated that chloroquine is superior to the control treatment in inhibiting the worsening of pneumonia, improving lung imaging findings, eliminating the virus from the body, and shortening the duration of the disease.
These claims are exciting. However, the report provided virtually no evidence in support of the claims.
Another study is more encouraging. It was conducted by an excellent group of scientists in southern France, a region hard hit by COVID-19. This, also, was not a randomized trial. Instead, the scientists compared 26 patients who received hydroxychloroquine to 16 who did not: after six days, the virus was gone from the body in 70% of those given the treatment, compared to only 12.5% of those who weren't. The drug appeared to be as effective in the sickest patients as in the least sick, but the study was too small to be sure about that. The study also was too small to say confidently that people who received the treatment were protected against a prolonged illness or death.
In summary, there is some reason for optimism that hydroxychloroquine may be effective in treating people with COVID-19. There are many studies underway, and we should have more solid answers within a few months.